ACHILLES TENDON RUPTURE SURGERY
What are the goals of surgery for an Achilles tendon rupture?
Regaining Achilles tendon function after an injury is critical for walking. The goal of Achilles tendon repair is to reconnect the
Bruising caused by an Achilles tendon rupture
calf muscles with the heel bone to restore push-off strength.
Who can have Achilles repair surgery?
Those best suited for surgical repair of an acute or chronic Achilles tendon rupture include healthy, active people who want to return to activities such as jogging, running, biking, etc. Even those who are less active may be candidates for surgical repair. Non-operative treatment may also be an option. The decision to operate should be discussed with your foot and ankle orthopaedic surgeon.
When should I avoid surgery?
You should not have this surgery if you have active infection or unhealthy skin at or around the site of the Achilles tendon rupture, or if you are not healthy enough to undergo surgery. Other concerns include diabetes, smoking, sedentary lifestyle, steroid use, and inability to follow postoperative instructions. Any health concerns should be discussed with your foot and ankle orthopaedic surgeon.
What happens during the surgery?
The surgical repair of an acute or chronic rupture of the Achilles tendon typically occurs in an outpatient setting. This means the patient has surgery and goes home the same day. Numbing medicine is often placed into the leg around the nerves to help decrease pain after surgery. This is called a nerve block. Patients are then put to sleep and placed in a position that allows the surgeon access to the ruptured tendon. Repair of an acute rupture often takes somewhere between 30 minutes and one hour. Repair of a chronic rupture can take longer depending on the steps needed to fix the tendon.
How will my foot and ankle orthopaedic surgeon repair the rupture?
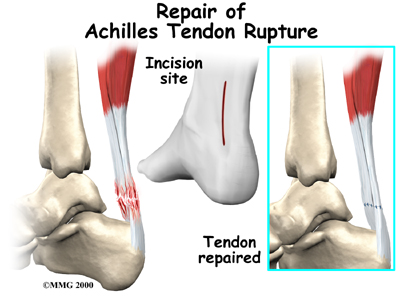
There are a variety of ways to repair an Achilles tendon rupture. The most common method is an open repair. This starts with
Above, the surgeon finds the torn Achilles. Below, sutures hold the torn ends of the Achilles together.
an incision made on the back of the lower leg starting just above the heel bone. After the surgeon finds the two ends of the ruptured tendon, these ends are sewn together with sutures. The incision is then closed.
Another repair method makes a small incision on the back of the lower leg at the site of the rupture. A series of needles with sutures attached is passed through the skin and Achilles tendon and then brought out through the small incision. The sutures are then tied together. The best surgical technique for your Achilles rupture will be determined by your foot and ankle orthopaedic surgeo.
What happens after surgery?
After surgery, the patient is placed in a splint or cast from the toes to just below the knee. Typically the patient will not be allowed to walk or put weight on the involved leg. Crutches, a walker, knee scooter or wheelchair are used to allow the patient to remain mobile. Patients are encouraged to keep the operated leg elevated above heart level to decrease swelling and pain.
If a nerve block has been given, patients can expect the numbing sensation to last from eight to 24 hours. For some people, a “pain pump” may be placed that delivers numbing medication over one to three days.
Patients are typically seen in the office two weeks after surgery. The splint or cast is removed and the surgical incision is evaluated. Stitches are usually removed at this time if they need to be removed at all. From two weeks to six weeks, the postoperative protocol varies based on surgeon preference. Patients may be allowed to begin weightbearing in a walking boot. Ankle motion is often allowed and encouraged. A cast is sometimes used instead of a boot.
At six weeks patients are usually allowed full weightbearing out of the cast or boot. Physical therapy is started and is aimed at restoring ankle range of motion. Strengthening of the calf muscles and Achilles is gradually allowed as the tendon heals. Patients are usually able to return to full activity by six months. It may be over a year before a patient achieves full recovery.
What are the potential complications?
There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots.
Potential complications specific to Achilles tendon surgery include wound infection and delayed wound healing. Re-rupture can also occur. There may be scarring of the tendon or thickening of the surgical scar. A nerve that gives sensation to the outside part of the foot can be stretched or injured during surgery, which can result in numbness or burning.
Frequently Asked Questions
What is the likelihood of success with the procedure?
Acute repairs usually do well. It is important to understand that even after a successful surgical repair the ultimate strength of the leg will likely be less than it was before the injury.
What is the risk of tendon re-rupture?
The risk of re-rupture after surgical repair is less than 5 percent. If re-rupture occurs, the tendon can be repaired again either directly or with other techniques that utilize other tissues and materials to reinforce the repair. Revision surgery is always more complex that the original surgery.